Expert

Jill Williams
Actions
Type
Topic
- Economic Impact
- Workforce
Tags
The Missouri Hospital Association’s 2023 Workforce Report finds that in 2022, there was a slight easing of the record-high vacancy and turnover rates experienced in 2021. This decline occurred in aggregate, as well as within the staff nurse segment of the workforce.
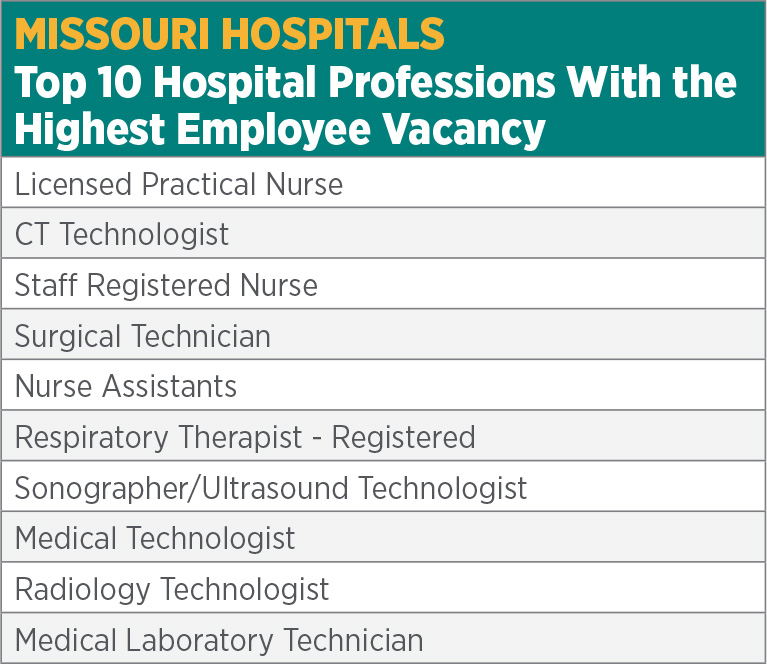
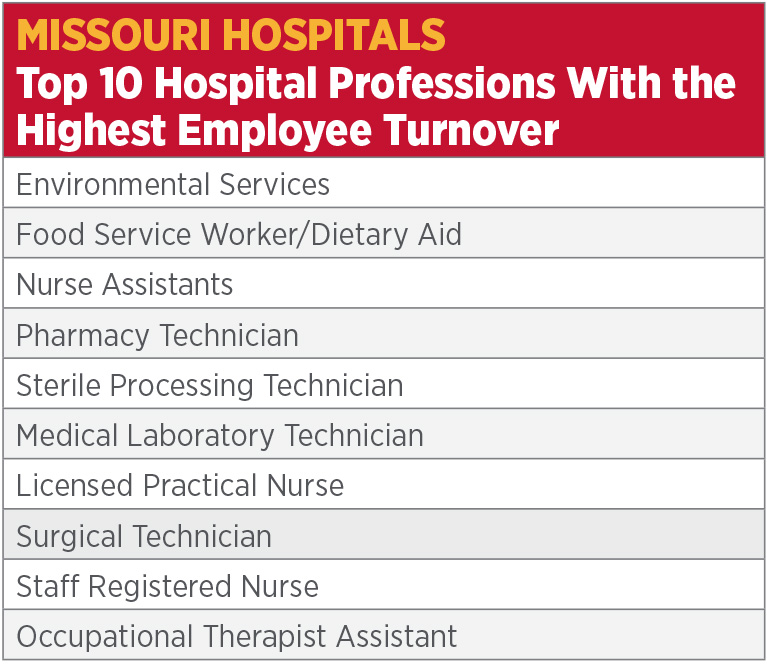
Although this relief is positive, the rates of vacancy and turnover experienced in 2022 still were much higher than historical rates. This year’s report finds a nearly one-quarter turnover rate among all surveyed positions statewide, with more than 40% for environmental services and dietary workers. The turnover rate among staff nurses — the largest single cohort of hospital employees — reached nearly 20%. This rate of flux within the health care workforce affects operations, cost and culture.
Although these workforce issues currently create a challenging environment, they also are long term and structural. According to the U.S. Bureau of Labor Statistics, the health care delivery system will need 2.6 million more workers nationally in the next eight years to accommodate demand, even as shortages persist today.1 In Missouri, an additional 64 full-time faculty positions would be necessary to accommodate all nursing school applicants who are qualified for admission. Presently, qualified nursing school applicants are turned away because of an insufficient number of faculty. Moreover, without additional investment or innovative approaches to nurse training, the education system will struggle to replace the 98 Missouri nurse educators who are expected to retire within the next five years.
Opportunities exist to mitigate these challenges. Hospitals continually are working to attract new staff, retain the incumbent workforce, and expand and retool the skills of other hospital team members. Bringing back workers who have left the hospital environment as caregivers, helping future health science instructors receive the credentials to educate the health care workforce and upskilling workers in their current specialty can help bridge the existing challenges. In the long term, more workers will be needed, and hospitals will need to create the cultures and operational flexibilities necessary to attract and retain the next generation of the health care workforce.
Every Missourian has a stake in the strength of the hospital workforce. These clinical professionals — and the many workers who support them — are essential to the delivery of emergency care, disease management and health improvement activities. State and local governments, academic institutions, businesses, and other partners can play an important role in mitigating the hospital workforce crisis.
The COVID-19 pandemic laid bare the immediate and long-term structural challenges in the health care workforce. Even if these historical rates of vacancy and turnover continue to recede, investments in the workforce will be necessary to deliver the workers needed to provide care in the future. Hospitals and all stakeholders must promote and reduce barriers to entry for health professions. At the same time, hospitals must ensure they remain employers of choice in the communities they serve to attract employees of all skill levels. This will require investment, flexibility and innovation.
2023 Statewide Report
A printable Workforce Report also is available.
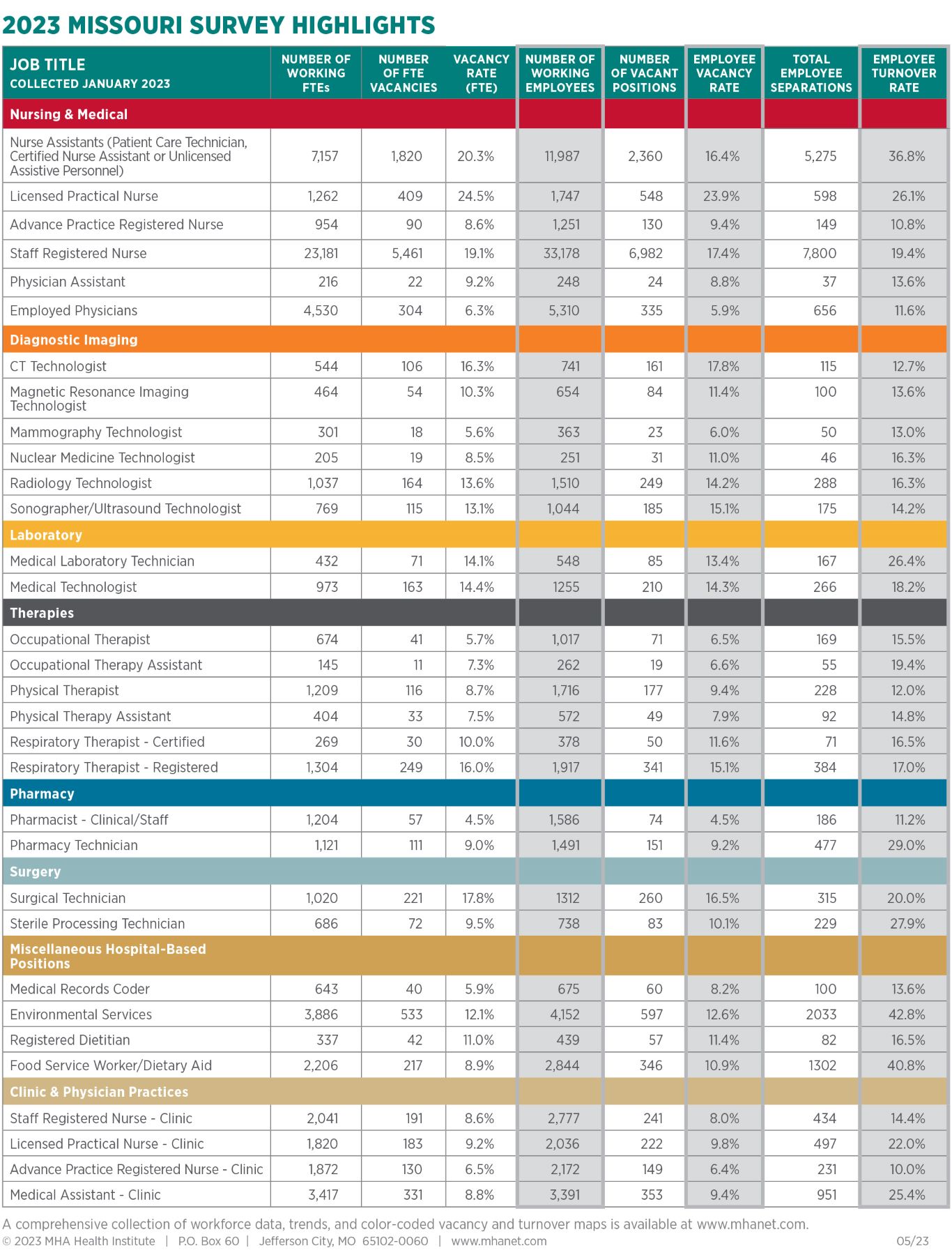
The report includes data from 128 hospitals and identifies trends among 28 hospital-based positions and four clinic and physician practice positions.
2023 Regional Reports
- Central
- Kansas City
- Northeast
- Northwest
- Ozark
- South Central
- Southeast
- Southwest
- St. Louis
- West Central
Also available is a workforce report specific to Missouri’s critical access hospitals. Missouri is home to 35 CAHs, and each submitted CY 2022 data for MHA’s 23rd annual workforce survey that focuses on turnover and vacancy rates both regionally and statewide.
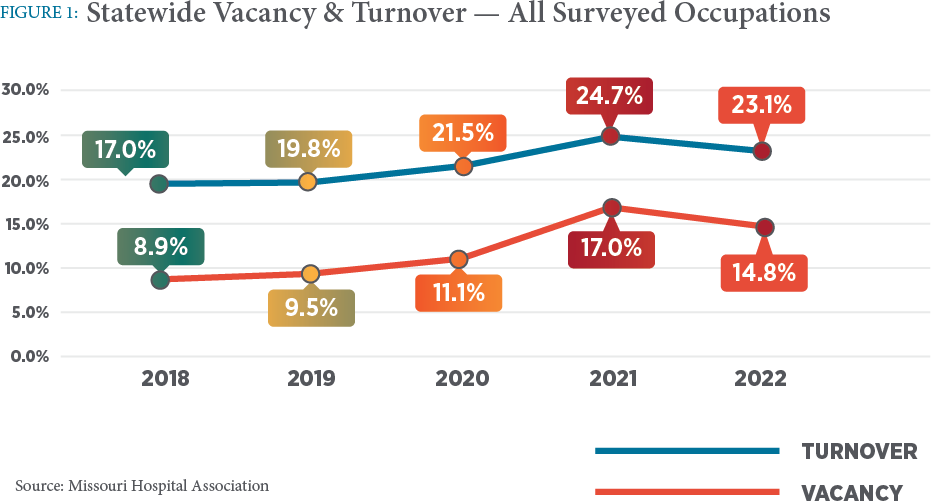
MHA’s 2023 Annual Workforce Report reflects Missouri hospitals’ workforce in 2022. The data indicate a small decrease from 2021 in vacancy and turnover rates among the majority of health care positions included in the survey. However, both turnover and vacancy rates among all surveyed professions remain significantly higher than pre-pandemic levels (Figure 1).
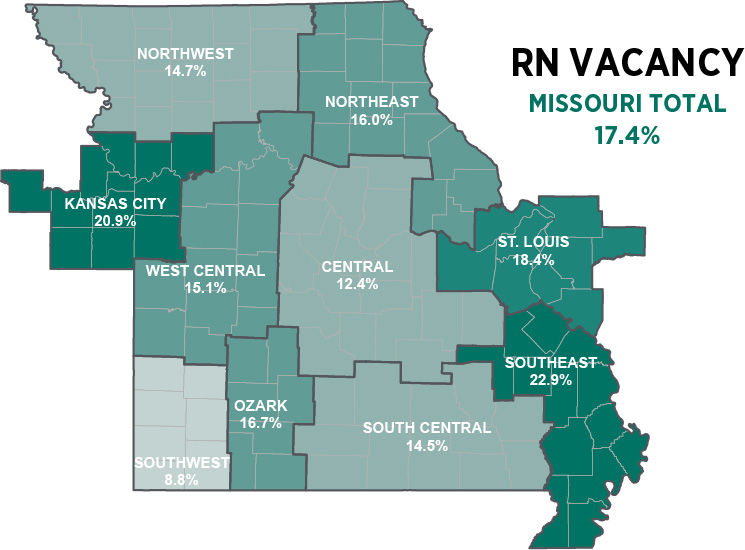
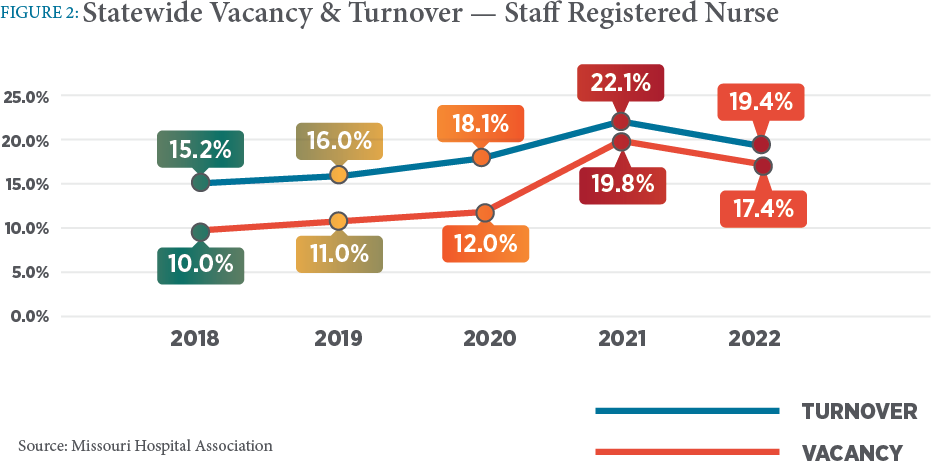
Staff registered nurses account for the largest single cohort of hospital employees in Missouri. This year’s report finds that staff nurse vacancy reached 17.4%. Although this number is a decrease from 19.8% in 2021, it reflects a notable increase from 11% in 2019 (Figure 2). According to the survey, Missouri has 33,178 nurses working in hospitals and 6,982 vacant staff nurse positions.
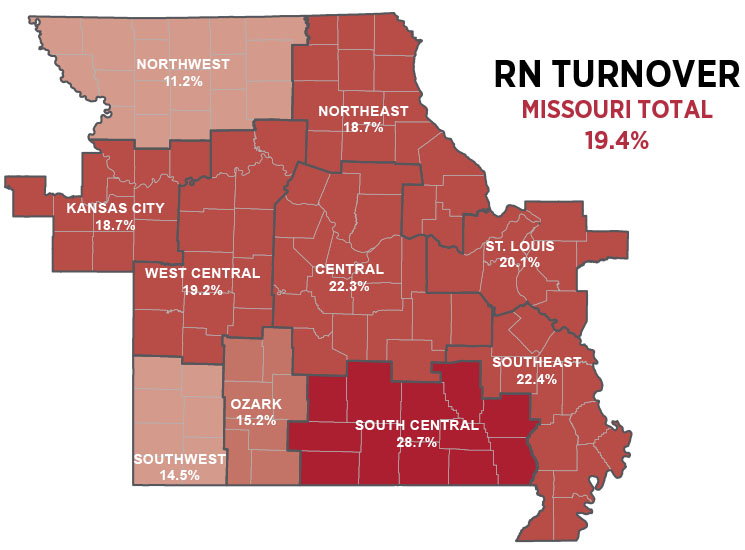
Staff nurse turnover is at 19.4% (Figure 2). This level of turnover is costly and disruptive for health care systems, and it can impact morale, disrupt the nurse and patient experience, and exacerbate an already pressing shortage of qualified talent. According to a study released by the National Council of State Boards of Nursing, the nursing shortage crisis will continue without concerted action. The study found that an estimated 97,000 RNs left the workforce during the past two years due to stress, burnout and retirements, and another 610,388 reported an intent to leave during the next five years.2
Several factors are leading to significant turbulence in the health care workforce, including an aging care-delivery workforce who are nearing retirement, the challenges of working in a highly dynamic and sometimes difficult environment, alternative work options for skilled professionals, among other causes. The workforce development community, including hospitals, has struggled to keep the pipeline for new employees sufficient to overcome the headway. At the same time, demand for care is growing.
Turnover is costly and has multiple impacts to hospitals. According to the 2023 National Healthcare Retention & RN Staffing Report published by Nursing Solutions, Inc., each percentage change in nurse turnover will cost/save the average hospital an additional $380,600 annually.3 Since 2020, one in five health care workers have quit their jobs, and as much as 47% of health care workers plan to leave their positions by 2025, according to a 2022 report by Definitive Healthcare.4 It is important for hospitals to identify turnover risks and understand how to address them.
Hospitals are reacting to the pressures that are placed on the workforce in multiple ways. Many hospitals have increased starting wages, are offering sign-on and retention bonuses, and are paying for more overtime hours to combat shortages and retain staff. However, wage adjustments have been eroded by inflation, reducing hospitals’ ability to keep pace. The result is a decrease in real-wage growth and slower benefit gains for employees. At the same time, hospitals are facing significant financial pressure overall. Reimbursement rates for care haven’t kept up with the cost of inflation. Costs — including labor — are driving a larger share of hospitals into negative operating margins.
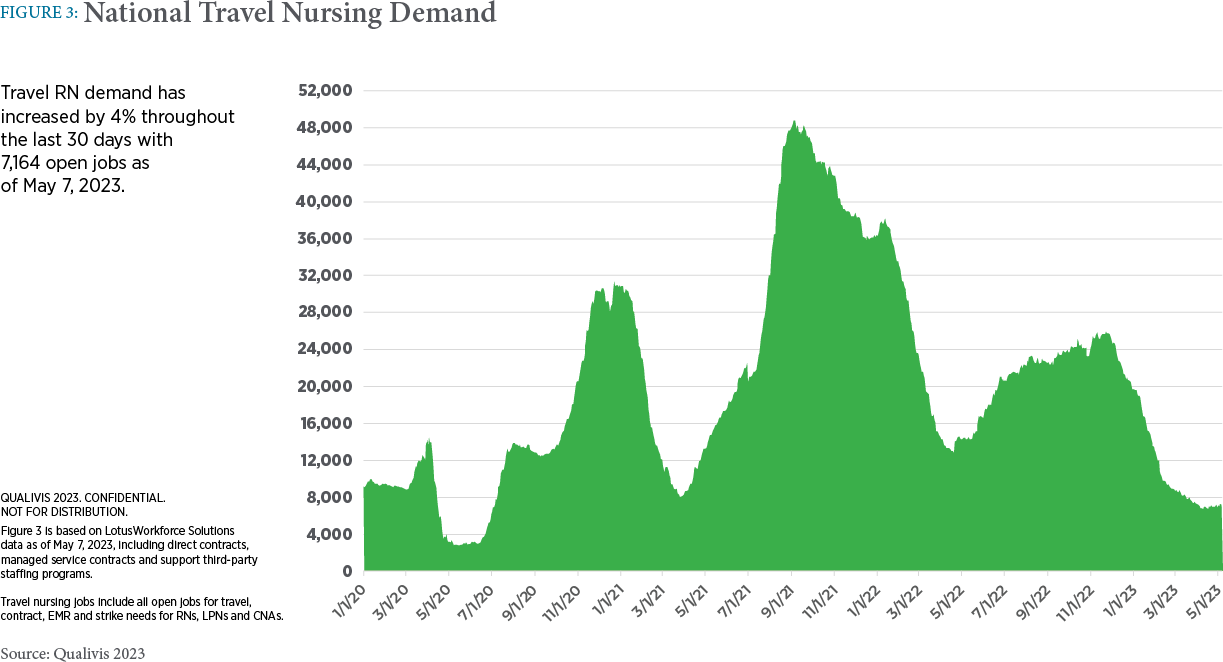
Fueled by the COVID-19 pandemic, demand for travel nurses skyrocketed in 2021 — increasing by a staggering 500%.5 As a result, many nurses made the switch to travel nursing to gain higher pay, flexible schedules and the opportunity to work in different locations. However, recent data from Qualivis suggest that the nationwide demand for registered travel nurses has returned to pre-pandemic levels. Nevertheless, Missouri remains one of the top states for travel nursing demand (Figure 3). Although necessary to address workforce shortages and surges in demand for care, agency staff can influence hospitals’ cultures and add significant costs to operations.
Structural challenges existed in the hospital workforce before the advent of the pandemic. COVID-19 amplified these challenges. Academic institutions are struggling to access necessary clinical rotations for student training resulting from hospital staff shortages. Similarly, instructor shortages are making it difficult for schools to accept all interested students.
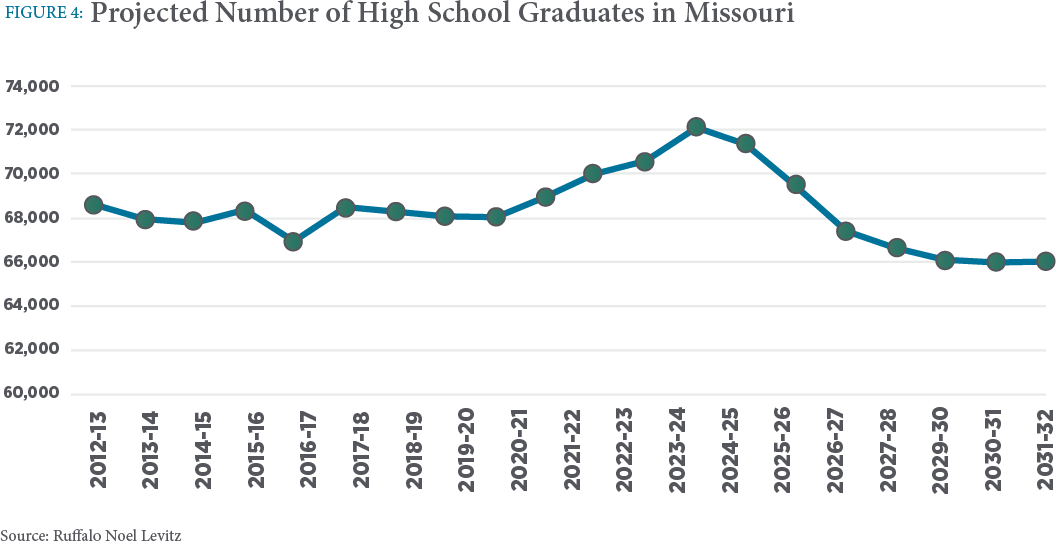
Reports suggest there will be a significant reduction in the number of high school graduates mid-decade. This will influence the ability of hospitals to recruit workers at all skill levels. Although not all hospital positions require a high school education, most clinical professions require high school and postsecondary education. These shifts could influence the population of candidates for future hospital and health care employment (Figure 4).
Nationally, community colleges were hit hard by the pandemic. Fall undergraduate enrollment began to stabilize in 2022 compared to fall 2021.6 However, postsecondary enrollment remains well below pre-pandemic levels. Missouri’s community colleges with programs for nursing and allied health are reporting that applications and enrollment are down by 50% from previous years. Nursing and health science programs continue to face challenges, including increasing program expenses, recruiting and retaining students, access to clinical training site space, sustaining small and specialized nursing and allied health programs, negative perceptions toward vocational/technical education, and finding qualified faculty. The Missouri Department of Higher Education and Workforce Development offers a Fast Track Workforce Incentive Grant to help individuals pursue a certificate, degree or industry-recognized credential in an area designated as high need. As of 2022, 46% of students were enrolled in allied health programs. Community and technical colleges are essential springboard institutions for careers in nursing and allied health professions.
Barriers exist for students as well, including transportation, housing, child care needs and academic preparedness. In addition, students may experience financial burdens related to tuition, equipment, fees, uniforms and other costs. Many nursing and health science programs have rigorous academic requirements and do not offer flexibility in course and clinical offerings that are conducive to those with family and financial obligations.
A comparison of the Missouri State Board of Nursing 2020 and 2021 annual reporting data suggest that Missouri nurse faculty shortages are more than critical. Qualified candidates willing to fill nurse faculty positions are limited. Throughout the past two decades, clinicians have helped fill some of the gaps in nursing education through dual roles as clinical staff and faculty. However, the impact of the pandemic on nursing practice, opportunities for nurses to earn much higher wages in clinical practice and compounded nurse burnout are leading to unprecedented challenges in their recruitment and retention.

Missouri’s nursing programs report that an additional 64 full-time faculty positions would be necessary to accommodate all applicants who are deemed qualified for admission. Unfortunately, these reports indicate at least 98 Missouri nurse educators plan to retire within the next five years (Figure 5).
Opportunities exist for academia and hospitals to address workforce shortages by partnering to explore creative faculty models to mitigate the educator shortage. These models include providing tuition reimbursement to help nurses return to school and pursue degrees to be educators, encouraging current nurses to work in a hybrid role as both nurse faculty and at the bedside, and encouraging retirees and individuals who have left the workforce to embrace nursing education as a way to give back to the future workforce.
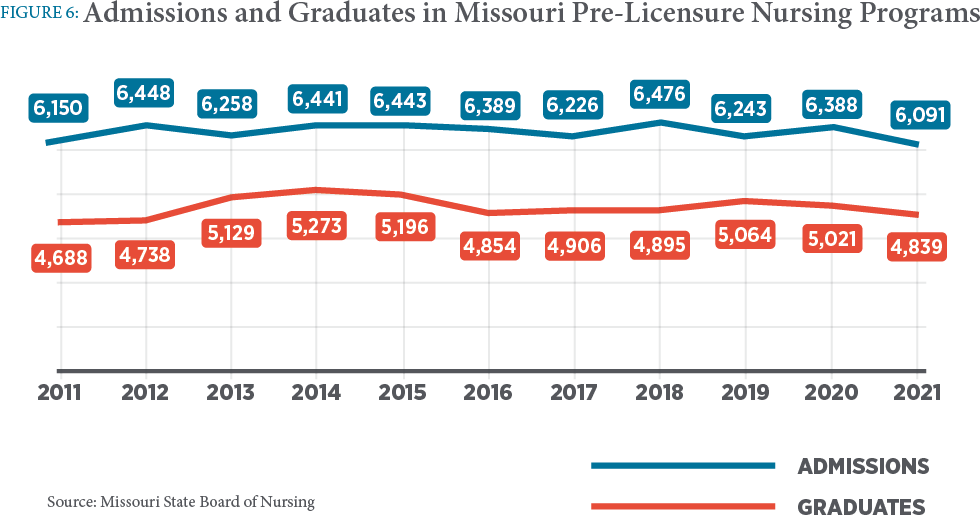
The Missouri State Board of Nursing 2022 annual reporting indicates that there are 10,224 students currently enrolled in nursing programs. There were 6,091 nursing students admitted in 2021; however, 1,221 qualified applicants were turned away (Figure 6). While some of these applicants may have applied to multiple schools, the number of qualified applicants that cannot be accommodated is too high given the demand within the profession.
State investment in the nursing workforce is creating new opportunities to reduce turnover and increase retention of nursing students. The academic-clinical partnership model helps hospitals hire senior-level nursing students as employees to earn a wage while meeting clinical objectives. Faculty still oversee the clinical experiences, but the students are paired with an experienced nurse where they work while gaining their required clinical learning. Many are hired on a permanent basis after graduation. This makes the transition from student to licensed nurse easier and decreases orientation time.
This model is one example of new and innovative programs funded by Missouri’s Nursing Education Incentive Program. Since its inception in 2011 and including the current 2023 grant awards, the NEIP has contributed more than $10 million to nursing education in Missouri. In 2022, a separate State of Missouri grant project provided an additional $3 million to nursing programs in Missouri. During the 2023 legislative session, lawmakers included $5 million in state funding to continue and extend the scope of the program.
As this report outlines, health care organizations are experiencing significant workforce challenges and are seeking innovative ways to address them. It is vital for hospitals to find effective strategies for attracting and retaining top talent within their organization.
MHA is committed to helping hospitals innovate to build a sustainable workforce. Although there are challenges, there also are opportunities. Programs that expand the professional pipeline, invest in training and career advancement for current employees, expand workplace flexibilities and care delivery models, and enhance support and protection for health care workers are essential to this innovation.
Pipeline Development and Recruitment
It is imperative that hospitals and their academic, community and government partners continue to collaborate on innovative ways to address workforce gaps. Working in partnership with local secondary K-12 schools is essential for building interest and exposing students — and their parents as influencers — to health career opportunities. This can occur through meaningful job shadow and work-based learning experiences, identifying and offering loan repayment programs, or connecting with local high school HOSA-Future Health Professionals chapters and Area Health Education Centers. Keeping students connected to the hospital by moving them into an entry-level role before or soon after they graduate from high school where they can work and further their education at the same time is an excellent way to attract and retain them.
The Missouri Chamber of Commerce, Missouri Department of Elementary and Secondary Education, and Missouri Hospital Association partner annually to host a Virtual Health Career Day. This important collaborative event shares the variety of opportunities that exist in health professions and provides a glimpse into hospital work with students and teachers. In 2023, more than 8,500 students and 450 educators and counselors participated in the event.
To attract talent, hospitals must take a multifaceted approach — starting from within. This includes recruiting a diverse talent pool; evaluating barriers to hire; focusing on skills-based hiring; creating a streamlined recruiting and onboarding process; retaining relationships with alumni; and offering earn while you learn, apprenticeship-style training programs.
Retention and Engagement
Retention and engagement of the current workforce must remain a top priority. Hospitals need to convey to front-line workers and leaders how much their work and commitment is valued. That means putting an emphasis on flexibility, work-life balance, recognition programs, purposeful rounding, and inclusivity and belonging. Frequent and consistent compensation reviews and stay interviews, and including worker voices in decision-making, can strengthen employee engagement and retention within the organization. Hospitals also can help by learning more about the challenges faced by their existing workforce and how to support them through roadblocks, including but not limited to lack of transportation, child and elder care, food insecurity, or housing.
Work Redesign
Many health care workers have complex work arrangements and are demanding more scheduling flexibility to accommodate family responsibilities. Some hospitals are working toward integrating flexibility into jobs and providing remote work where possible. Emerging staffing models are offering more shift options, variable start times and durations of shift work, app-enabled self-scheduling, and incentives to work less-desirable shifts or during periods of high demand. This includes internal staffing models that offer premium pay and flexibility with the benefit of staying with a single hospital or health care system.
Hospitals and health systems are deploying various staffing models and technologies to supplement the workforce. These include team-based models, virtual nursing, telehealth and artificial intelligence. By rethinking the role of the health care worker and the use of technology, hospitals may be able to unburden staff and improve efficiency, productivity and satisfaction.
Several Missouri health systems have adopted innovative systems and technology to bridge gaps in staffing. This includes scheduling systems that allow workers to identify shift openings that fit their schedule and nonwork demands. This “gig employment” model allows hospitals to use existing staff as internal agency staff, increasing flexibility for the incumbent workforce while reducing the need for and costs of external agency staff.
Professional Development
Ongoing professional development is essential for hospitals to embrace new, innovative ways to work — on the front lines of care and organizationwide. Hospitals can encourage opportunities for career advancement by evaluating skill sets and creating flexible, meaningful career pathways for entry-level roles. Developing talent through cross-functional training, service on interdisciplinary teams, stretch assignments, mentorship programs and succession planning has many benefits to the organization. These systems allow hospitals to identify the next generation of leaders and hone their skills. Leadership development training can help managers become more effective leaders, better communicate with their team members, build trust, adapt to change and drive innovation within their organization. Developing current talent should be a core business function that is focused on creating a culture where employees feel valued by having the opportunity to grow and thrive.
Well-Being and Safety
Hospital leaders are concerned about the well-being of their teams. The pandemic resulted in significant stress on health care workers as they were at the leading edge of pandemic care. Studies suggest the pandemic contributed to increased incidences of post-traumatic stress disorder, depression and anxiety among health care workers. This has caused some health care workers to leave the profession, making an already critical labor shortage worse. To better care for and retain staff, health system leaders must normalize help-seeking behavior, provide mentorship to less experienced nurses, and build support systems and training to help leaders and staff identify and address well-being. Organizations not only must support team member resilience, but give them a voice in addressing workflows and processes that may impede their work. Maximizing patient care is essential to reinspiring nurses to find the joy, satisfaction and meaning they value so highly.
What happens in the community can manifest in the hospital environment. This includes violence. Workplace violence has a significant negative impact on well-being, further contributing to burnout among health care professionals. In a recent survey, the American Nurses Association found that 58% of respondents considered their workplace unsafe.7 The U.S. Bureau of Labor Statistics indicates that of the 37,060 private sector workers who experienced trauma from nonfatal workplace violence in 2020, 23% worked in health care and related fields.8 Nationally, health care providers are four times more likely to be assaulted in the workplace.9 Recent findings published by Press Ganey indicate two nurses are assaulted in the U.S. every day.10
To reduce added stress from the environment, hospitals can build and leverage listening forums to elevate issues and act quickly on findings, provide training, enforce policies for protection of staff in the workplace, have clear pathways for addressing stress incidents, and reduce incivility and horizontal violence. Missouri does not have a mandated requirement for workplace violence reporting, a statewide tracking program or data aggregation system. However, MHA is leading an initiative to capture data on the prevalence of violence in health care settings and is collecting occurrence information utilizing the International Association of Healthcare Safety and Security standardized measures and categorization for aligned benchmarking, assessment and program refinement.
METHODOLOGY
A total of 128 Missouri hospitals participated in this year’s survey. The survey requested data on 28 hospital health care positions, and four clinic and physician practice positions. Responses are collected by the Missouri Hospital Association. Data are reported as of Dec. 31, 2022.
REFERENCES
1 U.S. Bureau of Labor Statistics. (2022, September 8). Occupational Outlook Handbook. Healthcare Occupations. Retrieved from https://www.bls.gov/ooh/healthcare/home.htm
2 Martin, B., Kaminski-Ozturk, N., O’Hara, C. & Smiley, R. (2023). Examining the impact of the COVID-19 pandemic on burnout and stress among U.S. nurses. Journal of Nursing Regulation, 14(1) 4-12. doi: https://doi.org/10.1016/S2155-8256(23)00063-7
3 NSI Nursing Solutions, Inc. (2023, March). 2023 NSI National Health Care Retention & RN Staffing Report. Retrieved from https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf
4 Popowitz, E., Bellemare, T. & Tieche, M. (2022, October). Addressing the Healthcare Staffing Shortage. Definitive Healthcare. Retrieved from https://www.definitivehc.com/sites/default/files/resources/pdfs/Addressing-the-healthcare-staffing-shortage.pdf
5 Kusterbeck, S. (2022, November 8). Travel Nursing Demand Is Waning: Now Hospitals Want Full-Time Nurses Back. Nurse.com. Retrieved from https://www.nurse.com/blog/travel-nursing-demand-waning-hospitals-want-full-time-nurses/
6 National Student Clearinghouse Research Center. (2023, February 2). Current Term Enrollment Estimates: Fall 2022 Expanded Edition. Retrieved April 2023 from https://nscresearchcenter.org/current-term-enrollment-estimates/
7 Levine, D. (2022, October 5). Tackling Health Care Burnout. U.S. News & World Report. Retrieved from https://www.usnews.com/news/health-news/articles/2022-10-05/tackling-health-care-burnout
8 U.S. Bureau of Labor Statistics. (2022, November 21). The Economics Daily. Workplace violence: homicides and nonfatal intentional injuries by another person in 2020. Retrieved May 4, 2023, from https://www.bls.gov/opub/ted/2022/workplace-violence-homicides-and-nonfatal-intentional-injuries-by-another-person-in-2020.htm
9 The Joint Commission. (2018, April 17). Sentinel Event Alert. Physical and verbal violence against health care workers. Retrieved from https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_59_workplace_violence_4_13_18_final.pdf
10 Press Ganey. (2022, September 8). On average, two nurses are assaulted every hour, new Press Ganey analysis finds. Retrieved from https://www.pressganey.com/news/on-average-two-nurses-are-assaulted-every-hour-new-press-ganey-analysis-finds/