- Ensure effective and structured communication tools are used.
- Host leadership safety briefs and huddles, and post notes on intranet or other staff communication channels within two hours.
- Expect unit level safety briefs and huddles.
- Expect debriefs to occur.
- Encourage and expect front-line decision making.
- Execute leadership rounding.
- Practice observational monitoring.
Expert

Jessica Stultz
Actions
Type
Topic
- Process Improvement
- Quality and Safety
Tags
Hospital leaders who choose to establish a high reliability organization (HRO) embark on a mission to commit to zero harm and realize true, purposeful work in health care.

Applying high reliability concepts in an organization does not require a huge campaign or a major resource investment. It begins with leaders at all levels thinking about how the care they provide could be safer. A commitment to support and sustain a system of high reliability principles and safety should be an organization’s overarching strategy. Culture is the foundation for vision and strategy.
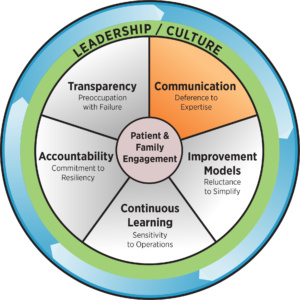
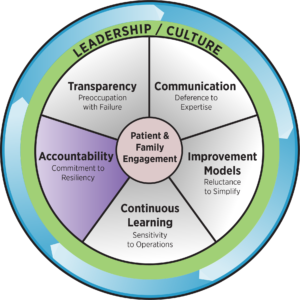
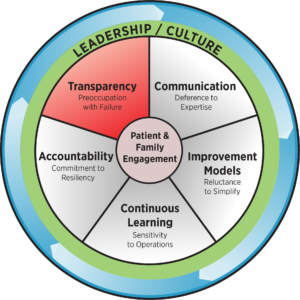
At the core of an HRO, there are five key principles, which are essential for any improvement initiative to succeed: deference to expertise, reluctance to simplify, sensitivity to operations, commitment to resilience and preoccupation with failure.
This online toolkit is designed to guide the process of transforming an organization into one where safe, timely, effective, efficient, equitable and patient-centered care is received by all patients. Each HRO principle and technique is described, along with practical application strategies and resources to guide organizations on their HRO journey.
Communication and Leveling the Power Differential
HRO Principle: Deference to Expertise
When confronted by a new risk, it is essential to have mechanisms in place to identify the individuals with the greatest expertise relevant to managing the situation. A high reliability culture requires staff at every level to be comfortable sharing information and concerns with others, and to be commended when they do. Leaders should listen and respond to the insights of staff who know how processes work at the point of care and the risks patients face. Without this transparent communication, a culture of high reliability is not possible.
Speaking up for safety entails the following.
- Anyone can ask questions without looking unwise.
- Anyone can ask for feedback without looking incompetent.
- Anyone can be respectfully critical without appearing negative.
- Anyone can suggest innovative ideas without being perceived as disruptive.
Achieving transparent communication requires a flat hierarchy and a strong learning environment that supports a climate in which people feel they can comfortably make suggestions. Effective teams develop communication expectations that lead to shared understanding, that anticipate needs and problems, and that use agreed-upon methods to manage situations – including those that involve conflict. In a culture that espouses teamwork and communication in the pursuit of safe, reliable and effective care, team members explicitly give permission to hold each other accountable across a flat hierarchy.
Improvement Models
HRO Principle: Reluctance to Simplify
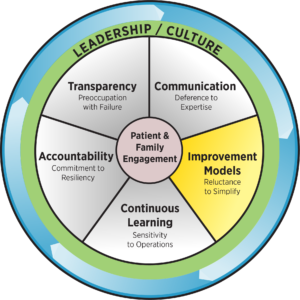
While simplifying work processes is highly desirable, it is risky to oversimplify explanations of what has happened or what might happen in the future. Being able to identify the often-subtle differences among safety risks may make the difference between early and late recognition. Simple processes are good, but simplistic explanations for why things work or fail are risky. Avoiding overly simple explanations of failure is essential to understand the true reasons patients are placed at risk.
Health care cultures that are highly reliable understand that their systems may fail in ways that have never happened before and that they cannot begin to identify all the ways in which their systems could fail in the future. One component of this principle involves using standard improvement tools to enhance work processes and patient outcomes. HROs build diverse teams and use the experiences of team members who understand the complex nature of their field to continually refine their processes. Sometimes improvements are initiated in response to a defect; however, HROs focus on preventing problems before they arise by deeply understanding the processes of care and operations. Once defects are identified, a systematic approach enables teams to redesign processes and achieve outcomes that matter to patients, families and staff.
Continuous Learning
HRO Principle: Sensitivity to Operations
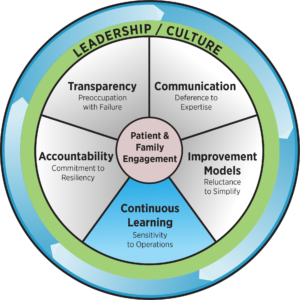
Keeping situational awareness is important for staff at all levels, because it is the only way anomalies, potential errors and actual errors can quickly be identified and addressed. Maintaining constant awareness by leaders and staff of the care delivery process is essential. This awareness is key to recognizing risks and working to prevent them.
Sensitivity to operations and continuous learning entails the proactive and real-time identification and prevention of defects and harm. Organizations need to be aware of errors occurring and correct them before they reach the patient. More time and focus should be placed on being proactive rather than reactive. Nurturing a more reliable culture requires continuous feedback loops in the form of data and insights to prompt action learning and outcomes. HROs exist in complex environments that depend on multi-team systems that must coordinate for safety. The safety of a hospitalized patient depends on the effective coordination and ability of physicians, nurses, pharmacists, medical technicians, aides, IT, support staff and many others.
Accountability
HRO Principle: Commitment to Resiliency
Despite the best efforts and past safety successes, health care errors will occur. Organizations with a highly reliable culture quickly contain errors, creating the ability to function despite setbacks. Leaders and staff should be trained to perform quick situational assessments and must be prepared to respond when system failures do occur.
Resiliency in hospitals stem from accountable staff. HROs hold people accountable for their actions, but not for flaws in processes or systems. Individuals are responsible to embody organizational values and, in return, the organization is responsible for treating individuals fairly and justly when things go wrong. A commitment to resiliency involves constructing systems in a reliable fashion that take human factors into account. They make it hard to do the wrong thing and easy to do the right.
Four components for making systems and processes more reliable over time include the following.
- Standardize – Design processes so that people do the same thing the same way every time. Standardization makes it easier to train people on the processes, and it becomes apparent if the processes fail, and where they fail, enabling the organization to better target improvement.
- Simplify – The more complex something is, the less likely it is to be successful. Staff may avoid following processes that are too difficult or time-consuming, which presents opportunities for mistakes. Simplified processes make it easy for people to do the right thing.
- Reduce autonomy – Health care professionals historically have been autonomous, making decisions based on personal preference or an individualized belief. However, this can result in care variation and less consistent outcomes. To achieve greater reliability, organizations must set the expectation that care delivery follows evidence-based best practices, unless contraindicated for specific patients, and the contraindications are then documented.
- Highlight deviation from practice – Clinicians sometimes have good reasons for departing from standardized processes. Smart health care organizations create environments in which clinicians can apply their expertise intelligently and deviate from protocols when necessary, but also relentlessly capture the deviations for analysis. Once analyzed, the new insights can lead to educating clinicians or altering the protocol. Both result in greater reliability.
Transparency
HRO Principle: Preoccupation with Failure
Health care cultures that are highly reliable start with recognizing that harm or error can occur at any time regardless of how long it has been since the last event. New safety risks may be developing, and unintended consequences can arise when changes are made. Even when celebrating improved quality, reliable cultures always are vigilant and look for what could have gone wrong to learn from it. Near-misses are viewed as evidence of systems that should be improved to reduce potential harm to patients, and they are opportunities to better understand what went wrong in earlier stages that could be prevented in the future. Transparently and openly discussing errors and near-misses supports the environment of HROs. Care should be taken to ensure these discussions remain systematic in nature and not devolve into finger-pointing. If staff feel they are being targeted, they will be reluctant to report future near-misses. Operational transparency exists when leaders, staff, patients and their families, organizations, and the community are able to visibly see the activities involved in the learning process. Having the courage to display work openly is a component of being an HRO. Transparency is the key to changing culture. HROs thrive on transparency and managing the unexpected. They are observant and focused on predicting and eliminating catastrophes rather than reacting to them.














