Expert

Dave Dillon
Actions
Type
Topic
- Population Health
Tags
That Lead To Poor Health Outcomes
Where an individual lives, works, learns and plays can have a significant influence on their health. However, very few of these factors transfer to a patient’s health record, limiting caregivers’ understanding of the nonclinical drivers of poor health.
According to researchers from the Hospital Industry Data Institute, the transition to a more robust health care coding system is enriching stakeholders’ understanding of how social determinants of health influence individual health and use of health care resources. Although collection and application of diagnosis codes related to SDOH remains in its infancy, the growing body of data suggest they have exceptional potential to help health care providers identify high-risk patients.
“Five factors, including policies, health services, behaviors, genetics and social circumstances, influence individual and population health,” said Mat Reidhead, Missouri Hospital Association and HIDI Vice President of Research and Analytics, and a primary author of the study. “Only 10% to 20% of these factors are affected by health services. The balance relates to nonclinical social and contextual circumstances surrounding the patient — your ZIP code typically predicts health more accurately than your genetic code.”
Understanding the major role nonclinical factors have on shaping patient health and care outcomes is essential. The 2015 transition to the International Statistical Classification of Diseases and Related Health Problems 10th Revision — commonly referred to as ICD-10 — created an opportunity to attach SDOH codes to patient records. ICD-10 includes 87 Z codes identifying patients with social circumstances, including housing instability, problems due to education and employment, psychosocial surroundings, socioeconomic status, and family and upbringing issues. An additional 13 Z codes capture other environmental risk factors, including difficulty in adherence to medical care, and adult abuse and neglect, among others.
In 2018, MHA’s first report on Z code reporting found that even with limited use of the codes, they provided exceptionally granular information on patients at risk of excess emergency room utilization due to social factors such as homelessness. These codes also showed solid predictive capability for health outcomes, which could support future reimbursement applications for nonmedical social support services that can significantly reduce health care spending.
This new body of work builds on those previous findings to help advance the understanding of facility and clinician awareness and use of the codes – looking specifically at various hospital departments and types of patients and payers.
“Although the percent of patients identified with social risk factors remains small, the research identifies several important connections between the care environment and the likelihood of coding for SDOH,” Reidhead said. “Emergency rooms, for example, are a common source of health care for low-income and socially complex patients. However, a relatively small percentage of ER patients are diagnosed with the SDOH Z codes, possibly due to the limited amount of time the physician has with the patient.”
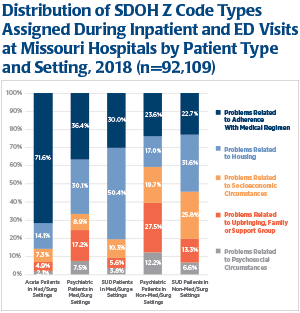
Venue and type of SDOH codes were correlated in the research. Among acute care patients assigned a Z code, nearly 72% of the codes related to adherence with medical care. Although this code was high among psychiatric patients as well, housing stability — a code commonly associated with homelessness — was a close second among the psychiatric population.
“A number of factors may explain the higher rate of SDOH coding among behavioral health patients,” said Alan W. Greimann, Executive Vice President of Compass Health, and President & CEO of Royal Oaks Hospital in Windsor, Mo. “Behavioral health care often results in a longer length of stay and includes a more holistic examination of the intersection of psychological and physiological aliments. In addition, health insurers require certain validation for care programs and payment related to the acuity of need, and authorize care related to that level of acuity. As a result, caregivers are required to address social complexities that influence individuals’ physical and behavioral health challenges.”
The HIDI analysis found psychiatric and substance use disorder patients were four-to-five times as likely to have one or more Z codes included in their patient record. These patients made up just 6% of all hospital visits but accounted for 38% of visits with an SDOH Z code assigned to a claim.
Length of stay and venue influence coding for SDOH. Researchers found that children’s and psychiatric hospitals coded for SDOH at higher-than-expected rates, while rural critical access hospitals and post-acute care hospitals are coding at a lower-than-expected rate. Finally, traditional hospitals — where 86% of all discharges occur —likely underreport SDOH codes by at least 4%, and perhaps at higher rates.
“Social factors play an outsized role in an individual’s health. Better coding for social determinants will underpin risk modeling, care improvement and health at both the individual and population health level,” Reidhead said. “The Z codes on social risk offer an important opportunity to identify the nonclinical drivers of poor health, and solid data is the first step in effectively allocating the clinical- and community-based resources needed to improve health and reduce costs.”









