1 Krupnick, M. (2020, December 21). Despite High Demand For Nurses, Colleges Aren’t Keeping Up. NPR. Retrieved from https://www.npr.org/2020/12/21/947496118/despite-high-demand-for-nurses-colleges-arent-keeping-up
2 Zhang, X., Lin, D., Pforsich, H. & Lin, V. W. (2020). Physician workforce in the United States of America: forecasting nationwide shortage. Human Resources for Health, 18(1), 8. doi: 10.1186/s12960-020-0448-3
3 Missouri Economic Research and Information Center. (2020, December). Missouri Workforce 2020 Employer Survey Report. Retrieved from https://meric.mo.gov/media/pdf/missouri-workforce-2020-employer-survey-report
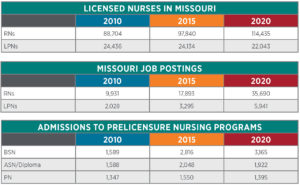
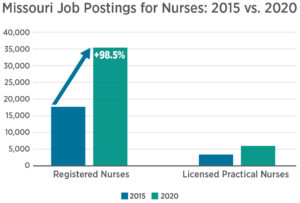
4 Missouri Division of Professional Registration, Board of Nursing. (2020). Annual Reports: 2010, 2015, 2020. Retrieved from https://pr.mo.gov/nursing-publications.asp
5 American Association of Colleges of Nursing. (2020, June). FY 2019 State Sheet: Missouri. Retrieved from https://www.aacnnursing.org/Portals/42/Policy/State-Resources/Missouri.pdf
6 Hawryluk, M. & Bichell, R. E. (2020, November 24). Need a COVID-19 Nurse? That’ll Be $8,000 a Week. Kaiser Health News. Retrieved from https://khn.org/news/highly-paid-traveling-nurses-fill-staffing-shortages-during-covid-pandemic/
7 American Hospital Association. (2020, May). Hospitals and Health Systems Face Unprecedented Financial Pressures Due to COVID-19. Retrieved from https://www.aha.org/system/files/media/file/2020/05/aha-covid19-financial-impact-0520-FINAL.pdf
8 Missouri Hospital Association. (2020, April). FAQ: COVID-19 and Use of Telemedicine Services. Retrieved from https://www.mhanet.com/mhaimages/COVID-19/FAQ_telehealth.pdf
9 Alexander, A., De Smet, A. & Mysore, M. (2020, July 7). Reimagining the postpandemic workforce. McKinsey Quarterly. Retrieved from https://www.mckinsey.com/business-functions/organization/our-insights/reimagining-the-postpandemic-workforce
10 Gatz, J., Porth, L. & Barclay, K. (2020). Mid-Response Assessment: Missouri Hospitals’ Response to the COVID-19 Pandemic. Missouri Hospital Association. Retrieved from https://web.mhanet.com/media-library/mid-response-assessment-missouri-hospitals-response-to-covid-19-pandemic/
11 Beck, M. (2020, March). Emergency Staffing Considerations (PowerPoint). MU Health Care. Retrieved from https://www.mhanet.com/mhaimages/COVID-19/Emergency%20Staffing%20Considerations.COVID19.March%202020.pdf
12 Estes, M. L. & Wagstaff, T. W. (2020, March). Burnout in Health Care. Trustee Insights. American Hospital Association. Retrieved from https://trustees.aha.org/burnout-health-care
13 American Hospital Association. (2020, December 8). How to Help Clinicians Stay Resilient during COVID-19. Retrieved from https://www.aha.org/aha-center-health-innovation-market-scan/2020-12-08-how-help-clinicians-stay-resilient-during-covid
14 Tannenbaum, S. I., Traylor, A. M., Thomas, E. J. & Salas, E. (2020). Managing teamwork in the face of pandemic: evidence-based tips. BMJ Quality & Safety, 30(1), 59-63. doi: 10.1136/bmjqs-2020-011447
15 Nguyen, M., Waller, M., Pandya, A. & Portnoy, J. (2020). A review of patient and provider satisfaction with telemedicine. Current Allergy and Asthma Reports, 20(11), 72. doi: 10.1007/s11882-020-00969-7
16 Boston-Leary, K., Brewington, D., Burns, H., et. al. (2020, December). Imagining the Post-COVID Nursing Workforce. HealthLeaders Exchange. Retrieved from http://promos.hcpro.com/pdf/SOCTelemed_CNOX20_Report.pdf?spMailingID=18326861&spUserID=MzkwNjcxNDI4Njg2S0&spJobID=2041472046&spReportId=MjA0MTQ3MjA0NgS2
17 Gold, M., Brainerd, E. & Francis, C. (2020, May). Driving Connection & Engagement in a Remote Workforce. Arthur J. Gallagher & Co. Retrieved from https://www.ajg.com/us/news-and-insights/2020/may/driving-connection-engagement-in-remote-workforce-in-covid-19/
18 Render, D. (2019). Millennial Myth-Busting: Harnessing Next-Gen Insights to Transform the Workplace. HR Pulse Magazine. American Society for Health Care Human Resources Administration. Retrieved from https://www.ashhra.org/millennial-myth-busting-harnessing-next-gen-insights-transform-workplace