Expert

Mat Reidhead
Actions
Type
Topic
- COVID-19
- Population Health
Tags
The Disproportionate Impact of COVID-19 on Black and African American Communities in the St. Louis Region
Executive Summary
Throughout the U.S., stakeholders are attempting to make sense of the differences in health outcomes related to COVID-19 among disparate communities and populations. To draw meaningful conclusions, analysis of the limited data surrounding the novel virus warrants a lens that is nuanced by an understanding of how individual and communitylevel social determinants of health affect COVID-19 trend lines. Furthermore, there is a need to identify the most salient protective factors related to risk of exposure to COVID-19 and account for the cultural-historical contexts of disparate communities within regions.
Understanding the disproportionate impact of the disease on Black and African American communities is an important first step toward disentangling the complex causal pathways between upstream social determinants of health and downstream health outcomes. While understanding the association between neighborhood composition and COVID-19 will assist policymakers in near-term decisions on resource allocations, as more robust data emerge around the novel virus, further analyses must incorporate a more holistic approach to the complex deterministic role of underlying social factors.
This research brief aims to quantify COVID-19-related health disparities in the St. Louis region using ZIP code-level data on confirmed cases and demographic composition. Mirroring racialized COVID-19 trends in other metropolitan areas, the report focuses on observed, yet unexplained, disparities in the prevalence of confirmed cases among predominantly Black and African American communities in the St. Louis region. This research is not intended to extend dated narratives linking race alone to observed differences in health outcomes, as responses to such narratives may distract attention from the more impactful levers to promote public health and well-being. This report concludes with recommendations for future research and action steps that enable prevention, mitigation and healing.
A Joint Publication From:
- Missouri Hospital Association
- Alive and Well Communities
- Center for Health Economics and Policy
- St. Louis Department of Health
- Saint Louis County Department of Health
- Saint Louis Integrated Health Network
- Saint Louis Regional Health Commission
- Washington University School of Medicine
On April 8, 2020, Dr. Fredrick Echols, the City of St. Louis Health Director, reported that among the city’s nearly 500 cases, there had been a total of 12 fatalities — all of which were among African American residents in a city that is 46% white.
As the pandemic continues to spread across the country, these initial data are being validated by reports from New York, Detroit and Chicago suggesting that the burden of morbidity and mortality from COVID-19 has been disproportionately borne by people of color and individuals living in poverty. Understanding these local patterns is critical for designing policy and public health interventions to reduce the spread of disease broadly, as well as to specifically address its disproportionate impact on vulnerable populations.
While data on the race and ethnicity of individuals with COVID-19 across Missouri are currently not publicly available, local public health agencies in the City of St. Louis, in addition to St. Louis, St. Charles, Jefferson and Franklin Counties, are reporting confirmed cases by ZIP code of residence. Prior studies have shown that ZIP code of residence is highly correlated with a number of social determinants of health — defined as the conditions in which people are born, grow, live, work and age. For many health conditions, an individual’s ZIP code is as predictive of their health outcomes as their genetic code; however, there has thus far not been a systematic examination of issues related to race and social determinants of health in the context of the COVID-19 outbreak in the state. The aim of this research brief is therefore to quantify COVID-19-related health disparities in the St. Louis region using ZIP code-level data on cases and demographic composition.
DATA
This analysis includes data on confirmed COVID-19 cases and racial composition for 113 ZIP codes across the St. Louis region, defined as the City of St. Louis, St. Louis County, St. Charles County, Jefferson County and Franklin County. Data on confirmed cases were gathered from each local public health agency in the region on April 13, and again on April 20, 2020. On April 13, there were 2,681 combined cases in the region as reported by the included LPHAs. One week later, on April 20, the number of cases had grown to 3,859, marking a one-week, 44% relative increase. On April 20, the range of confirmed COVID-19 cases varied from
0 in seventeen ZIP codes to 677 per 100,000 residents in 63113, The Ville neighborhood in North St. Louis City.
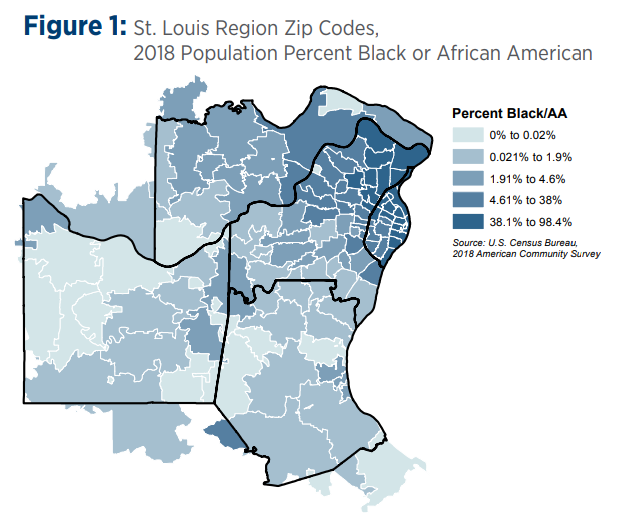
Demographic data on the racial composition and population density of each ZIP code were gathered from the U.S. Census Bureau’s 2018 American Community Survey, five-year estimates. Across the region’s 113 ZIP codes, the percent of the population identifying as Black or African American ranges from 0% to 98.4% (Figure 1) while population density ranges from 10.6 to 9,267 residents per square mile.
ANALYSIS
St. Louis regional ZIP codes were stratified by the percentage of the total population being Black or African American, and evaluated by the number and incidence of confirmed COVID-19 cases on April 20, the one-week change in the number of confirmed cases from April 13, and the proportion of regional cases compared to the proportion of regional population. The association between confirmed cases and population density also was evaluated to ascertain the possibility of variation in COVID-19 incidence between ZIP codes being explained by the physical proximity of residents. Due to the limited number of observations, this analysis was restricted to bivariate cross tabulations and descriptive statistics.
Research on health disparities in the St. Louis region demonstrate the relationships between specific social determinants of health, race, community context and health outcomes. Qualitative regional data and the emerging quantitative data about racial identities of patients should be reconciled. Absent a blending of qualitative and quantitative data, community context, and an accounting for historical actions that lead to the current milieu of a community, the racialization of COVID-19 data can reproduce health narratives and public health responses that further stigmatize Black and African American people and marginalize communities. Those narratives run the risk of perpetuating a story that connects disease to Blackness and Black culture rather than naming and disrupting the trajectory of cultural-historical and contemporary internal and external social factors that shape Black communities and resident health.
RESULTS
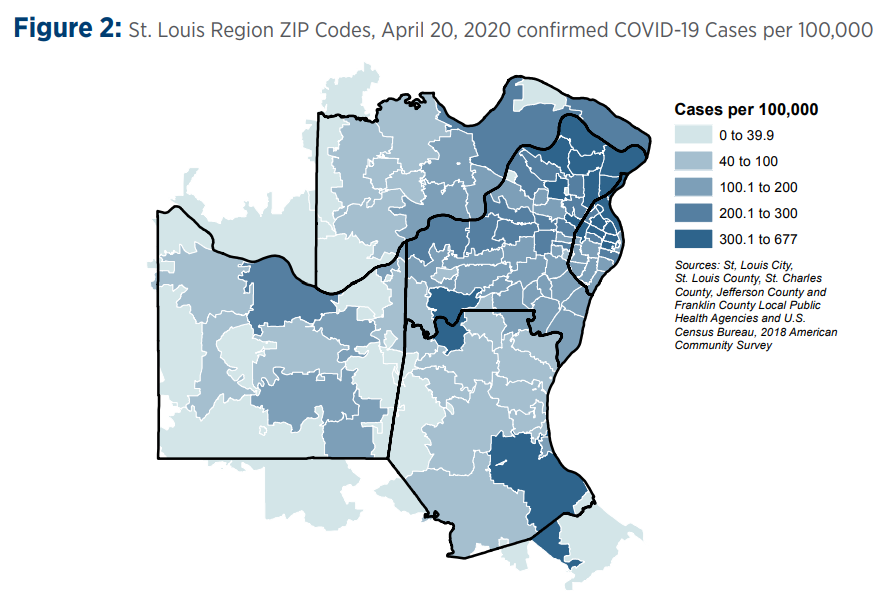
As a rate of the population of each ZIP code in the St. Louis region, confirmed COVID-19 cases were largely clustered in communities in North St. Louis City and County on April 20, 2020 (Figure 2).
Organizing ZIP codes into groups that categorized the proportion of the Black or African American population in each ZIP code at less than 5%; between 5% and 50%; and over 50%, revealed that the region’s 19 ZIP codes with a majority Black or African American population had a combined rate of COVID-19 cases near 400 per 100,000 residents, while the 68 ZIP codes with fewer than 5% Black or African American residents had 127 cases per 100,000 residents on April 20, 2020 (Table 1). Taken as a whole, ZIP codes with a majority Black or African American population accounted for 16% of the region’s population, but 34% of its confirmed COVID-19 cases. Additionally, the one-week percent change in confirmed cases from April 13 reveals that the number of cases in majority Black or African American communities grew at twice the rate of communities with the smallest Black or African American populations — 63.7% versus 29.3% (Table 1).
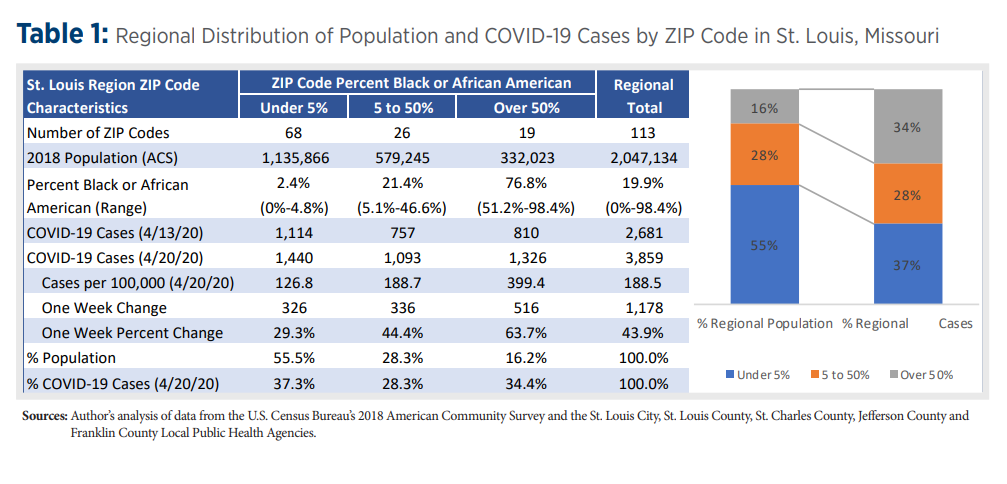
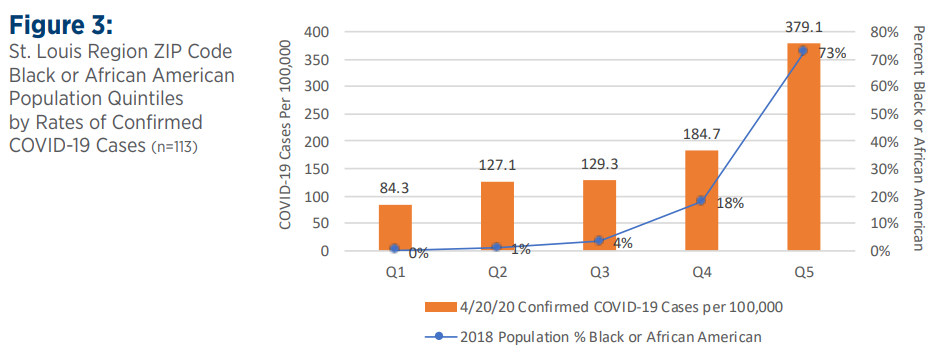
Stratified by quintiles, the 23 regional ZIP codes with the fewest Black or African American residents had 84 confirmed cases per 100,000 on April 20, while the 23 ZIP codes with the largest percentage of Black or African American residents had a rate of 379 per 100,000 residents, or 4.5 times the rate of confirmed cases in the first quintile ZIP codes (Figure 3).
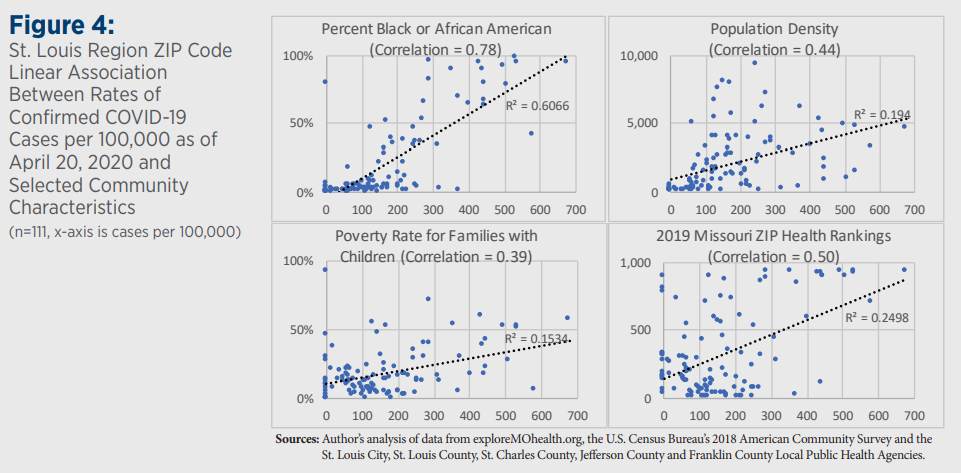
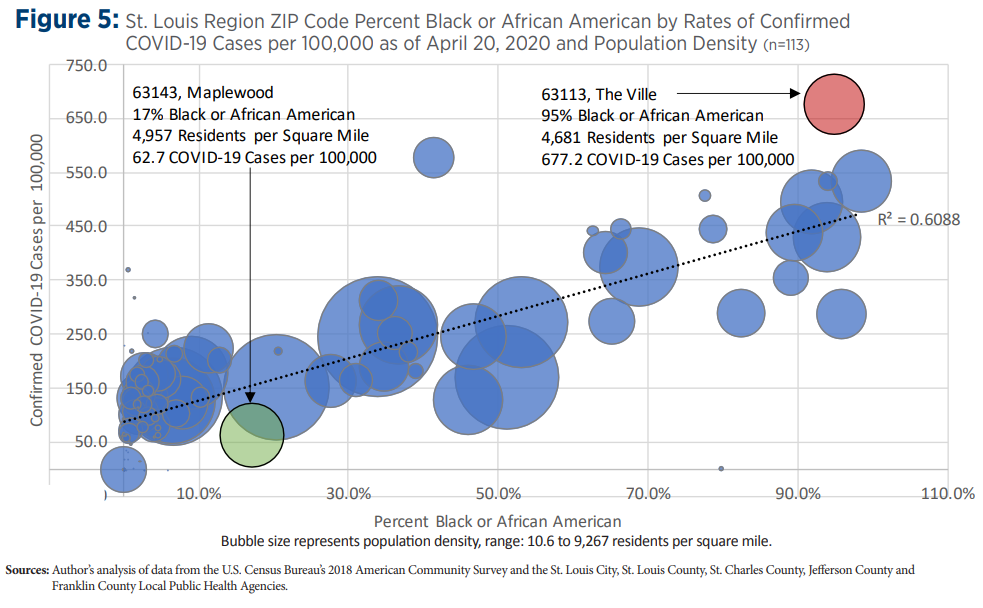
At the same time, compared to regional poverty rates, ZIP Health Rankings and population density, race appears to be the strongest linear predictor of confirmed COVID-19 cases per 100,000 residents among ZIP codes in the St. Louis region (Figure 4). One illustrative example is to compare Maplewood and The Ville: two locations with similar population density and separated by only 3 miles, yet with a ten-fold difference in the rate of confirmed COVID-19 cases on April 20, 2020 (Figure 5).
While additional research can help ascertain causes, immediate policy action also is needed to begin to address disparities for communities disproportionately impacted by this pandemic. The results presented here support the need for individual and neighborhood-level data collection, intervention and policy considerations such as directing enhanced education, awareness, testing and contact tracing resources, conducted in a culturally responsive manner, to the most impacted communities in the St. Louis region. For example, to address limited awareness and misperceptions about COVID-19 in the African American community, PrepareSTL, a region-wide communication campaign, was established March 17, 2020. Funded by the Missouri Foundation for Health in partnership with the Regional Health Commission, the City of St. Louis, St. Louis County and other community health organizations, PrepareSTL deploys community health workers and other community volunteers to provide culturally appropriate messages on how to mitigate COVID-19 while remaining physically, emotionally and economically secure.
That communication initiative was followed by an expansion of COVID-19 testing sites in African American neighborhoods, such as The Ville. Identification of testing sites was guided by health department geocoded maps documenting clusters of COVID-19 cases within predominantly African American communities in North St. Louis City and North St. Louis County. Additionally, because current testing criteria prioritize individuals with severe symptoms, directing testing sites to areas with high prevalence of chronic conditions known to exacerbate COVID-19 was imperative.
Ongoing tracking of outcomes among Black and African American individuals in St. Louis also is crucial. National data from the Centers for Disease Control and Prevention suggests that in addition to observed community-level differences in confirmed cases, there are stark disparities for Black and African American individuals in terms of hospitalization and case fatality rates.
COVID-19 could prove to be a catalyst for the medical community in embracing the importance of social determinants of health. While the disproportionate impact of COVID-19 on communities of color is refocusing national attention on ubiquitous health disparities for Black and African Americans, longer term solutions are needed to address structural barriers to health and well-being.xi All solutions to address racial disparities are urgently needed and need to be systems-oriented, community-driven, and guided by the unique social and historical context of race in the St. Louis region. Immediate and long-term interventions should focus on public health and trauma-responsive approaches that prioritize prevention of harm from the virus and the negative impact of social determinants, mitigating the impact of the external and internal social factors that act on the Black community, and repair of harm by allocating resources that promote healing according to the Black communities.