Actions
Type
Topic
- Advocacy
- State Legislation
Tags

The 2021 Legislative Guide summarizes MHA’s positions on anticipated state legislative issues.
The guide identifies critical advocacy agenda items for the upcoming session and can be used to support and inform hospital-based advocacy efforts at the state level. A printable Legislative Guide is available.
President’s Letter
Every legislative session offers challenges and opportunities, but the 2021 legislative session promises to be a watershed year.
The 2020 legislative session was cut short, as legislators adjourned during the state’s shut-down at the beginning of the COVID-19 pandemic. The General Assembly adapted to remote work and was able to return to Jefferson City to finalize budgets and other legislative priorities. The legislature returned in the fall for two special sessions, only to see one of those sessions cut short, as many members of the General Assembly and their staff tested positive for COVID-19.
It’s this backdrop that will usher in the 2021 legislative session. Key for hospitals will be our efforts to support initiatives to sustain our pandemic response. Not only will the Missouri Hospital Association be involved in law and regulatory initiatives to support care and ongoing surges, the association also will be working on long-term reforms, including turning existing waivers into permanent program changes.
Concurrently, we will work with policymakers and others to implement the Medicaid expansion ballot measure adopted by the state’s voters in August 2020. When fully implemented, expansion is expected to provide more than 200,000 Missourians with better access to quality health care. We will strive to ensure that Missouri’s Medicaid program becomes not only bigger, but better.
With the economic downturn caused by the COVID-19 pandemic, the state’s budget is expected to be challenging. Also, Medicaid “reforms” that would slash hundreds of millions of dollars from hospital payments likely will be debated. Medicaid’s hospital spending exerts little pressure on the state’s general revenue because of Missouri’s long-standing reliance on the hospital provider tax. Even so, increased spending often is cited as a political justification for payment cuts masked as reform. MHA is committed to transforming the Medicaid payment system in a responsible manner that creates a sustainable platform and enables hospitals to deliver high-quality health care to enrollees.
This Legislative Guide provides more details about MHA’s state legislative priorities, as well as some of the adverse proposals we’ll be working to block. With the political fallout from the Medicaid expansion ballot measure, we may see some fervent legislative attacks.
Effective advocacy in an ongoing pandemic will be a challenge. MHA will continue to be fully engaged with you as we represent your interests. We expect 2021 to be a momentous year in state health policy.

Herb B. Kuhn
President and CEO
Missouri Hospital Association
TRANSFORMING HEALTH CARE
Medicaid Expansion
On Aug. 4, 2020, Missourians voted to adopt a constitutional amendment to expand Medicaid eligibility, as authorized by the federal Affordable Care Act. The vote was a culmination of years of work by expansion proponents, including MHA and its members. It was a victory for all Missourians, but approval by the voters marks only the beginning of work to ensure that the proposal is implemented. The Missouri General Assembly must appropriate the money to enable Missouri state agencies to implement Medicaid expansion.
When fully implemented, Medicaid expansion will make coverage available to Missourians who are 19 to 64 years of age with an income level at or below 138% of the federal poverty level. More than 200,000 Missourians are expected to gain coverage.
The constitutional amendment calls for expanded coverage to begin July 1, 2021, which is the start of the next state fiscal year. It also directs the MO HealthNet Division to notify the Centers for Medicare & Medicaid Services of Missouri’s intent to implement expanded eligibility standards.
During the 2021 state legislative session, there likely will be challenges in securing legislative budget authorization for the expansion. However, the Parson administration appears to be working diligently on the details of implementation.
Medicaid Payment Reform and Transformation
State policymakers will continue to pursue Medicaid reform in 2021, and MHA will be fully involved in the process. MHA recognizes and appreciates that Medicaid payment reform, if done well, offers an opportunity to improve the quality, efficiency, capacity and value of care provided to Medicaid enrollees. There are ample prospects for improvement. Missouri should move away from payment systems based on obsolete data and uncertain projections. Instead, those systems should provide fair opportunity among hospitals to achieve equity of payment based on updated costs of care, efficiency, patient characteristics and patient outcomes. Building effective value-based reimbursement systems is a challenge, but one well worth undertaking.
The initiative offers potential promise and peril for hospitals, but MHA is well prepared. It has convened membership initiatives to discuss the “must-haves” and “can’t-haves” of Medicaid reform, and will continue to develop and refine evolving reform proposals based on member engagement.
The Medicaid transformation process is entering its third year under the leadership of
MO HealthNet Director Todd Richardson. Some of that reform work is occurring outside of the legislative arena. But several Medicaid reform initiatives were debated in the 2020 legislative session and are expected to resurface in 2021. They include the establishment of a fee schedule for Medicaid outpatient services and an effort to repeal the so-called “out-of-state” payment, which goes to Missouri hospitals that treat Medicaid enrollees from other states. The payment helps offset some of the unreimbursed cost of treating non-Missouri Medicaid patients and allows hospitals to get comparable payment for out-of-state Medicaid patients and Missouri Medicaid enrollees.
MHD’s proposal to convert outpatient reimbursement to a Medicare-based fee schedule faced stiff opposition from MHA in the last legislative session. MHA’s opposition focused on the proposed rate of reimbursement, which was pegged at 90% of Medicare’s outpatient payment rates and used the Medicare wage index for the Jefferson City labor market. An MHA contractor, Milliman, Inc., estimated that MHD’s proposal would trim Missouri hospital payments by $100 million. MHD did not offer a specific proposal to replace the out-of-state payment, although certain legislators did so in response to the division’s concern about the payment stream’s significant growth and skewed distribution. MHA opposes eliminating this payment stream without establishing an acceptable replacement. Both issues received serious debate last session, but ultimately, hospital advocacy and the emerging COVID-19 crisis forestalled changes.
Outpatient and out-of-state payment reforms are expected to come to the fore again in the 2021 legislative session. MHA is working with its members to coordinate advocacy messages and develop consensus around alternative proposals.
Managed Care Standards
Currently, most policy standards governing Medicaid managed care plans are established by contracts between MHD and the plans. Providers have little or no role in shaping these standards, as they would if they were created by and codified in law or regulation. In the 2021 legislative session, MHA will advocate for legislation clarifying that Medicaid managed care plans are subject to current state insurance laws governing patient protections that apply to health maintenance organizations in the commercial market.
Patient Boarding in Hospitals
Children in the custody of the Missouri Department of Social Services Children’s Division too often remain in hospitals after it is no longer medically necessary for them to be there. There are no acceptable discharge options. Allowing these children to be abandoned in hospitals is harmful to the child and costly to the hospital. MHA will sponsor legislation for the division to take physical custody of a child when it is no longer necessary for the child to be hospitalized. If the division fails to do so, it will be responsible for the costs of boarding the child.
IMD Waiver
The Missouri DSS appropriations bill for SFY 2021 included direction for MHD to pursue a waiver from CMS that would allow for Medicaid payments for adults residing in institutions of mental disease, or IMDs. The federal SUPPORT Act authorizes CMS to grant waivers of the “IMD exclusion,” and the Trump administration has been aggressive in approving states’ requests for them. Missouri’s waiver is being written by the Department of Mental Health, with help from the consulting firm Health Management Associates. MHA staff has been engaged and supportive of the effort. A waiver is expected to be published for public comment this winter, with submission to and subsequent approval from CMS coming in late spring or early summer 2021.
PROTECTING THE FRA PARTNERSHIP

State Budget Stresses
COVID-19 has made its mark on Missouri’s budget.
Deferral of the individual income tax filing deadline from April to July and an anticipated decline in revenue growth resulted in Gov. Parson withholding more than $450 million in state spending at the end of SFY 2020. These cuts were carried forward into the current fiscal year.
SFY 2020 revenue growth of 2.4% was budgeted (+$230 million); however, actual revenues for the year fell by 6.6% (-$633 million). The state’s budget office, the Office of Administration Division of Budget and Planning, has not issued an official revised estimate for the current state fiscal year, but historically, an updated “consensus” revenue estimate is agreed to by the administration and legislative budget writers in December in advance of the legislative session. The substantial federal stimulus money provided to state government appears to have eased revenue reductions, to some extent, in the early months of FY 2021. However, the ending of these programs, coupled with a second wave of COVID-19 infections, portend continued uncertainty and a risk for revenue shortfalls for FYs 2021 and 2022.
Medicaid has experienced substantial growth throughout the past seven months. In some measure, that is due to federal eligibility protections tied to federal COVID-19 relief funds. Additional federal funds from a temporary increase in the state’s Medicaid match rate largely will offset this growth but leave little for the state to use to fill other shortfalls.
Historically, revenue growth of $250 million to $350 million is needed just to keep pace with the growing costs of K-12 education, higher education, mental health services, corrections and Medicaid. This means that in a normal year, Missouri budget writers are confronted with difficult budget-balancing decisions. The potential for historic revenue reductions from the ongoing pandemic and uncertainty of future additional federal relief make the budget outlook for FYs 2021 and 2022 particularly austere.
FRA Partnership is Crucial
For nearly 30 years, Missouri hospitals have paid a provider tax called the Federal Reimbursement Allowance, or FRA. This public/private partnership with state government generates more than $2 billion dollars annually of matching federal funds. The FRA tax rate for hospitals far exceeds the tax rate of most Missouri businesses and is much higher than hospital taxes in most other states. The provider tax has freed up billions of general revenue dollars for other state priorities. The collapse of this tax would decimate the state budget and cripple funding priorities for education, mental health services and corrections. Preserving this long-standing partnership is crucial to ensure Missourians have access to quality health care while protecting Missouri’s fiscal health.
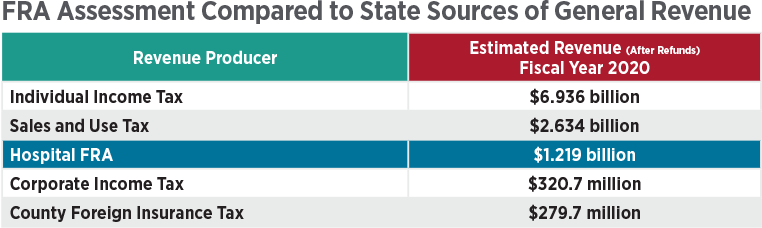
What is the FRA?
The FRA is Missouri’s hospital provider tax. It is a major source of state revenue, surpassing all but the two largest sources of state general revenue — the state sales tax and the individual income tax. In FY 2020, it produced nearly $1.2 billion, which was used to generate $2.3 billion in federal Medicaid matching funds for Missouri state government.
Role of the FRA
In the last completed fiscal year, each dollar of hospital FRA generated $1.91 in federal funds.
In 2018, the General Assembly enacted MHA-supported legislation to update and strengthen state laws, providing safeguards and accountability for the tracking and use of FRA funds and associated Medicaid hospital payments. The most recent report based on those laws verifies that in FY 2020, 85% of the state’s share of Medicaid hospital spending came from the FRA.
In FY 1990 before the FRA began, state general revenue funded 39.5% of all Medicaid spending. In FY 2020, the state general revenue percentage was 16%. This decline largely is because of the FRA and similar provider taxes for nursing homes and pharmacies.
Reauthorizing the FRA Laws
Because the state laws authorizing the FRA lapse on Sept. 30, 2021, they must be reauthorized during the 2021 legislative session.
The General Assembly has reauthorized the FRA provider tax laws 15 times since they first were enacted in 1992 as an initiative of the Ashcroft administration. For nearly 30 years, the FRA provider tax has enjoyed broad bipartisan support from both the executive and legislative branches of government. However, the FRA reauthorization bill sometimes is used as negotiation leverage in political maneuvering to advance some legislators’ political priorities.

PROTECTING PUBLIC HEALTH AND SAFETY
Responding to the COVID-19 Pandemic
In 2020, responding to the COVID-19 pandemic was all-consuming. Missouri hospitals collaborated intensely and well with state, local and federal governments to address myriad challenges. Those challenges include the financial free-fall associated with the loss of elective and most outpatient procedures during the spring of 2020, securing a sufficient supply of personal protective equipment and COVID-19 testing capacity, and removing regulatory and statutory obstacles, among many others. State government authorized 500 waivers of various state standards in 2020 to enable a more effective response to pressing COVID-19 needs. All of these actions helped sustain hospital operations and maintain access to the needed services.
Unfortunately, a resurgent pandemic is cascading into 2021. Hospitals will continue to need the same type of collaboration with state government to keep pace. If there is a positive aspect to the pandemic, it is that health care providers, regulators and patients have learned to use state and federal waiver flexibilities to improve the delivery of care, making it more affordable and accessible. MHA will pursue legislative efforts to incorporate those waiver flexibilities into state law. A prime example is to make permanent the expanded capacity to deliver services via telehealth technology.
COVID-19 Liability Protections
Hundreds of thousands of Missourians have contracted COVID-19, and thousands have died. The health care system and its clinicians are highly stressed from the demands of the pandemic. In such an environment, the General Assembly should create reasonable liability standards that stave off nonmeritorious lawsuits arising out of care delivered during a declared public health emergency.
Public Health Infrastructure
MHA’s and members’ efforts to coordinate with the public health system throughout the COVID-19 pandemic have revealed the effects of long-term underfunding and inadequacy of public health infrastructure, workforce and data systems. Missouri ranks 39 overall combining various measures of public health. By comparison, in the early 90s, Missouri was in the middle of all states in public health. This has been a gradual decline relative to other states throughout the last 30 years. Additionally, Missouri ranks 50th nationally in state and local public health funding. The national median is $33.50 per person, but Missouri spends $6 per person. Counting federal dollars, Missouri ranks 46th in the nation.
Furthermore, the existing variation of jurisdictional funding, authority and support limits the ability of the Missouri Department of Health and Senior Services to implement a statewide approach among 114 counties and the City of St. Louis.
Solving these long-term systemic problems is a daunting task. Solutions in a tight budget environment will be difficult — an incremental approach may be necessary. MHA will coordinate with our members and work with our partners in public health to support enhancements to the public health system.
Time Critical Diagnosis
MHA expects that legislation will be introduced to alter the state’s Time Critical Diagnosis System. This system is designed to provide timely and appropriate emergency medical treatment for people who suffer trauma, stroke and the potentially fatal form of heart attack known as STEMI (ST-segment elevation myocardial infarction). MHA engaged with its members to clarify their preferences regarding TCD laws and regulations. Based on those discussions, MHA supports creation of a TCD advisory committee and removal of duplicative peer review requirements for TCD. MHA will advocate to ensure that hospitals have a stronger voice on TCD standards; that the TCD System is a voluntary system where no data is required to be collected from nonparticipants; and that funding for the administration of the TCD System, including surveyor costs, is preserved.
Prescription Drug Monitoring Program
MHA will continue to support legislation to create a state prescription drug monitoring program comparable to the voluntary county-based model in place in many Missouri counties and cities. Such legislation would establish a common statewide standard. Among other benefits, a PDMP could help reduce opioid abuse caused by illicit drug-seeking or fragmented prescribing decisions.
Conceal and Carry in Hospitals
MHA opposes legislation that would allow concealed carry permit holders from Missouri or another state to bring their weapons into publicly accessible areas of a hospital. Currently, only security personnel and law enforcement can be armed within a hospital. The legislation would exacerbate demands on hospital security in their work to deescalate volatile situations in hospital settings. It is unclear how the bill would apply to patients with firearms who may be temporarily drugged or otherwise incapacitated. Also, some hospitals have invested significant sums in metal detectors and staff to keep firearms out of the buildings. Hospitals have suggested that allowing weapons into hospitals may encourage practitioners to practice in other states. It is not clear who would care for Missouri hospital patients in their absence.
AN EXCEPTIONAL WORKFORCE
In recent years, MHA has successfully promoted numerous proposals to aid hospitals in developing and retaining a quality workforce, and successfully opposed legislation that would interfere with hospitals’ ability to make physician employment and medical staff privileging decisions. In the 2021 state legislative session, MHA will advocate for several proposals.
Interstate Medical Licensure Compact for Physicians
Previously, MHA supported successful efforts to authorize Missouri’s participation in interstate licensure compacts for nurses, physical therapists, psychologists and emergency medical services personnel. These compacts promote expedited licensure of practitioners in participating states. In 2021, MHA is promoting a similar interstate licensure compact for physicians. The compact is expected to streamline and accelerate the process of securing licensure approval between states, as well as expand telehealth capacity.
Advanced Practice Registered Nurses
Advanced practice registered nurses are a vital part of the provision of high-quality health care. In response to the COVID-19 pandemic, various practice restrictions on APRNs were waived, including the requirement that an APRN practice with the collaborating physician continuously present for at least one month before practicing in a setting where the collaborating physician is not continuously present. Another waiver temporarily removed a geographic proximity limitation for the use of telehealth by APRNs outside of a rural area. These waivers have been vital to the provision of health care during the pandemic response and have shown the advantages of more flexible standards. During the 2021 session, MHA will promote legislation to make the waiver of these restrictions permanent.
MHA also will collaborate with several organizations to promote legislation to give APRNs greater authority to deliver health services under the auspices of a collaborative practice agreement with a physician. Missouri state law is more restrictive than most other states in this regard, which creates an incentive that runs counter to Missouri’s efforts to promote a robust workforce to support rural health. APRNs trained or practicing in Missouri know they can leave Missouri to practice with greater autonomy in many other states, including the states bordering Missouri.
In addition, MHA will continue its support of broader legislation to loosen physician supervision and other restrictions on the ability of APRNs to deliver health care services.
Pharmacy Regulatory Jurisdiction
There has been confusion as to whether DHSS can promulgate rules to set standards for the provision of pharmaceuticals in hospitals independent of the Missouri Board of Pharmacy.
This confusion has led to a lack of clarity in the role of pharmacy technicians in hospitals and the ability of hospital pharmacists to do remote verification. MHA will sponsor legislation to clarify regulatory jurisdiction regarding the delivery of pharmaceutical services in hospitals.
Covenants Not to Compete
MHA will continue to oppose legislative proposals that would limit hospitals’ ability to use covenants not to compete in physician employment contracts. Hospitals use these contractual agreements when recruiting a new physician to a practice or community. They ensure that the hospital has a reasonable period of time to recover the significant investment required to recruit and place the physician, and develop the practice. In accordance with court rulings, these contractual restrictions rarely last more than two years and often include the opportunity for the physician to “buy out” the covenant not to compete.
AUTHORIZING HEALTH SERVICES

Certificate of Need
During the 2020 legislative session, proposals were filed in the House and Senate to repeal state laws requiring certificate of need approval for new hospitals and the acquisition of a single piece of medical equipment costing more than $1 million. Historically, MHA has opposed repeal of the certificate of need laws but has supported certain modifications to them. In previous years, legislation was filed that would change the process by which CON decisions are made. For example, one bill would have replaced the legislator members of the Missouri Health Facilities Review Committee with gubernatorial appointees and prohibited ex-parte communications in the CON review process. MHA did not oppose these changes.
Consent to Treatment
MHA will monitor legislation that addresses who makes health care decisions for an incapacitated patient who does not have anyone with legal authority to make decisions for such patient. MHA has supported previous versions of this legislation and will work to ensure that any proposal that advances provides legal protection to hospitals and does not create an administrative burden.