Expert

Mat Reidhead
Actions
Type
Topic
- COVID-19
- Research
Tags
Hospitals’ Role In Identifying Comorbidities For Expedient COVID-19 Vaccine Distribution
The first dose of COVID-19 vaccine was administered in Missouri on Dec. 14, 2020. That was one down and roughly 12 million to go to fully inoculate the state’s entire population — the currently approved vaccines require two doses, and Missouri’s population is 6.1 million.
In reality, the portion of the population that will take up inoculation for COVID-19 is much less than 100%. First, the vaccines currently are approved for individuals older than 16 or 18 (depending on the manufacturer); second, conspiracy theories abound; and third, centuries of medical mistreatment toward disenfranchised populations in the U.S. has left primarily Black and Brown Americans with a natural mistrust of medicine — government-funded experimental medicine developed at warp-speed, notwithstanding.
A poll commissioned by MHA, and conducted last week, revealed that just 58% of Missourians were “very likely” or “somewhat likely” to want the vaccine when it becomes available to them (42% and 16%, respectively, +/-3.5% P≤0.05). Building trust in the safety and efficacy (not to mention existential import) of the vaccines among individuals with skepticism rooted at any level will be a monumental effort that already is underway in the Show Me State. These efforts must yield a portion of Missourians of sufficient size to induce “herd immunity.” A large portion of the adult population needs to trust the science and take up the vaccine, along with an invisible medal of meritorious civil service.
Vaccine coverage needed to induce herd immunity largely depends on how contagious the disease is —typically between 50% and 90% of the population needs to become vaccinated. Unfortunately, the novel SARS-CoV-2 coronavirus is so novel, we don’t yet know what the golden uptake ratio is. Assuming it’s around 70% of the population, that would mean 4.3 million Missourians would need to be vaccinated to restore normalcy. That would be nine in 10 adults ages 18 and older.
So, perhaps Dec. 14 was one down, 8.6 million to go. Nearly one month later, we’re at that minus 162,000. Arguably, this is the largest logistical challenge ever faced by elected bodies charged with protecting the health and safety of the populace in Missouri and elsewhere.
Wisely, Missouri has focused the early “Phase 1A” distribution of a scarce supply of vaccines to individuals who, if infected, would either threaten the stability of the health care system that we all need to thrive in the event we need care for any reason, or have a high probability of having an adverse reaction to the virus, such as hospitalization or death. Today, Missouri Gov. Mike Parson announced the second tier of Missourians eligible to receive the vaccines, including people with underlying health conditions that put them at high risk of adverse COVID-19-related outcomes in the “Phase 1B Tier 2” cohort.
Efficiently and expediently vaccinating a large group of geographically dispersed individuals with targeted conditions that can be difficult to verify will introduce a gauntlet of logistical hurdles. For example, and purely for illustrative purposes, how many Missourians between ages 40 and 64 have heart disease, diabetes, COPD or obesity — all risk factors known for adverse COVID-19-related outcomes? And then for logistical purposes, which areas of the state are situated most ideally to reach the largest number of these Missourians at the greatest speed? That’s where hospitals come in. Not only are they directly saving lives at the bedside, the historical data they generate by state statute carries the potential to indirectly save lives with bytes of insight.
For example, between 2019 and 2020, Missouri hospitals submitted 9.4 million inpatient, emergency department and outpatient clinic claims for 1.5 million Missourians between the ages of 40 and 64 to the Hospital Industry Data Institute. According to the Census Bureau, there are 1.9 million people in that age range, meaning 79% of all Missourians ages 40 to 64 visited a hospital or related clinic during the last two years.
So, the next question might be, for example, how many of them were diagnosed with heart disease, diabetes, COPD and obesity? The answer is 369,000; 276,000; 127,000; and 197,000, respectively. That’s roughly 970,000 Missourians, right? Wrong. And the key is the difference between the Boolean operator — “and” used in the first question, versus “or.”
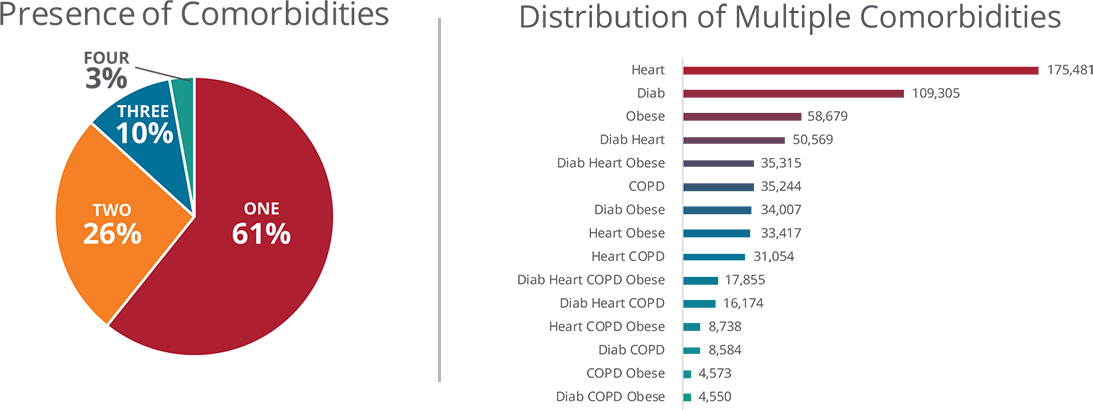
These conditions are not mutually exclusive, in fact, they’re correlated by causation — obesity is upstream of diabetes, which is upstream of heart disease, and so on. In fact, 39% of Missourians in this age range that visited a hospital were diagnosed with more than one of the four conditions (above). In other words, the question should be “how many of them were diagnosed with heart disease, diabetes, COPD OR obesity,” and the answer would be 623,545.
Accounting for the presence of multiple comorbidities reduces the challenge of projected demand. The next step is locating finite areas throughout the state where people, either in number or disproportionate burden, are living with these conditions and face a greater risk of hospitalization or death from COVID-19. Doing so would provide powerful decision support to public officials striving to optimize distribution strategies.
Hospitals are helping there, too, with geographic data that can be used to geolocate disproportionately impacted communities. For example, the highest concentration in the state of individuals ages 40 to 64 with one or more of these conditions is in the St. Peters community in St. Charles County — 1.3% of the 623,000 individuals identified with historical hospital claims data live in the 63376 ZIP code. Including the five surrounding ZIP codes encapsulates 5.2% of the entire priority group on a geographic footprint that is less than one-half of 1% of Missouri’s 69,704 square miles (below).

MHA and HIDI are eager to assist in minimizing the number of hurdles in this greatest of logistical gauntlets. Estimating the supply of at-risk recipients and where they might be most likely to seek out a vaccine is the easy part. Inducing demand by education and example will require influencers big and small, young and old in every single community throughout the state to commit to family, friends and neighbors to take up the civic duty, pin on the invisible medal and get us to that golden ratio. Then, we can all get back to work on improving our shared society while planning for a better rescue next time.









